Intro: Incremental AI assists to doctors will cascade into healthcare revolution
Five years ago, I was diagnosed with central sleep apnea. Apparently my brain sometimes forgets to remind my lungs to breath when I’m sleeping. While a diagnosis of central sleep apnea (CSA) doesn’t compare with cancer’s urgency or MS uncertainty, CSA’s short-term effects (headaches and bad dreams) and long-term implications (higher risk of neurological disorders) got my full attention.
My physician offered no cure. But recently, I spent 30 seconds searching Consensus.app, an AI tool that distills the wisdom of 200 million research articles, and learned about Diamox, a drug that is remarkably effective at reducing CSA. Though Diamox has been extensively studied, it’s largely ignored by the medical establishment, perhaps because it’s off-patent and lacks a highly motivated corporate champion.
Obviously, the press is full of stories about AI in medicine: AI is transcribing doctor’s notes from appointments, optimizing patient positioning for CT scans, analyzing millions of potential atomic structures for curative efficacy, and automating telehealth onboarding. It’s easy to forecast that AI will transform or obliterate the technology we use today to analyze and treat people, for example, as this analyst suggests, “vanquishing” pagers and fax machines over the next 25 years.
But each of those examples represent incremental rather than transformative changes. In each, AI displaces existing tech or grafts some new power onto an existing tool; each resembles taking a sail off a tall ship and replacing the lost power with an engine and screw propeller. Ships can move when the wind isn’t blowing, but the world doesn’t immediately change.
But, as with shipping, far bigger changes are ahead. Just as engine-powered ships eventually exploded the volume of global trade, spawned giant manufacturing complexes and sales channels, and gave consumers access to better, cheaper goods, accumulations of small changes wrought by AI will eventually cascade into entirely new categories of experience for health providers, medical institutions, and consumers. In hindsight, today’s medicine will look as archaic as a tall sailship.
Today, most of the emergent categories and experiences that AI will unlock are invisible. You might say they’re just glimmers in the marketplace’s eye; novel applications barely exist, consumers don’t yet know what to call the services or devices they crave, monetization models don’t exist, and the value chains and resellers that will eventually deliver the goods and services to the mass market also don’t exist. But if we look closely enough — for example at my experience with CS and Diamox — we see some visible hints of the radical changes ahead in healthcare’s fundamental structure and footprint.
Seeking a cure for CSA
As I mentioned above, recently I’ve been playing around with various AI tools that focus on medicine and healthcare. The tool that so far most impresses me is Consensus.app.
Consensus.app has digested and analyzed 200M+ academic papers and research studies in the Semantic Scholar database. From Consensus’s FAQs: “Consensus is an academic search engine, powered by AI, but grounded in scientific research. We use language models (LLMs) and purpose-built search technology (Vector search) to surface the most relevant papers. We synthesize both topic-level and paper-level insights. Everything is connected to real research papers.” The tool is available to the public, and searches are free.
That sounds very theoretical, so let’s dive into my own experience. I used Consensus to investigate a topic that strongly interests me: I suffer from central sleep apnea (CSA), which means that when I’m sleeping, my brain occasionally doesn’t remind my lungs to breathe. (Here’s the NIH on CSA.) Some days, I wake up with a headache, or I’m groggy in the middle of the day. My average blood oxygen saturation (SPO2) at night, as measured by my Fitbit, ranges between 93% and 96%, averaging 94% or 95% most nights. One other unpleasant symptom of CSA: on nights when my SPO2 average is low (which means it occasionally dips a lot lower) I sometimes startle awake out of an unhappy or angry dream. Maybe that’s my mind trying to create a story that explains its sudden oxygen-deprived state? Worse, though, sleep apnea significantly increases my risk of Alzheimers (by 28%) and Parkinsons (by 54%).
When I was diagnosed with CSA, I asked my doctor, a smart guy in his mid 40s whose site says he’s a “third generation internist,” if he recommended any medication. He shrugged and said no. (The NIH agrees, stating that all possible medications for CSA are “investigational” and “there is no approved pharmacological treatment for CSA.”) My doctor suggested I might try a CPAP machine, but noted that this technology is mostly studied for people with obstructive sleep apnea. Unfortunately, I used a CPAP for six months and a) it was a pain and b) didn’t move the needle for me.
I decided to test Dr. AI, asking Consensus: “Is there a drug that reduces central sleep apnea?” After 10 seconds, Consensus proposed three candidates, with extensive notes about their pros and cons. According to Consensus, the top candidate is acetazolamide, a drug often used by climbers to reduce altitude sickness. The drug, I learned, has been widely prescribed for glaucoma and heart disease since the 1950s.
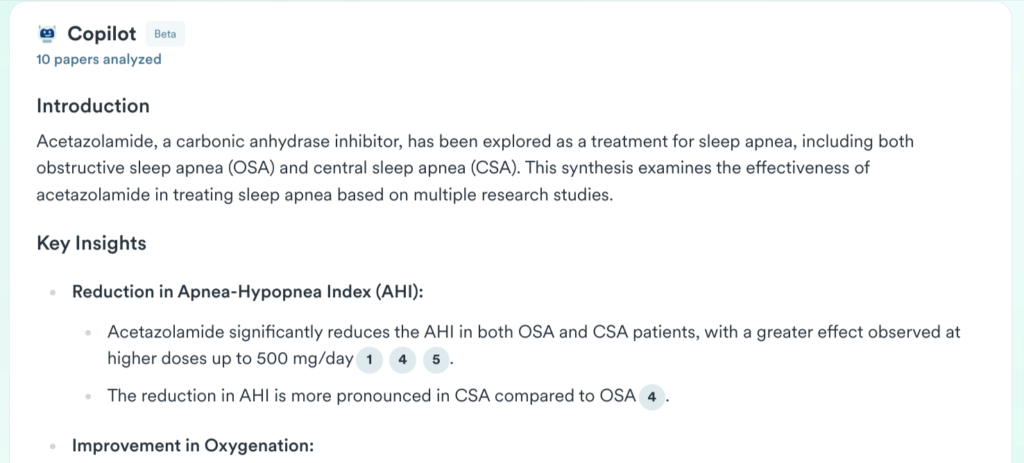
I asked Consensus.app for more information about acetazolamide’s effects on CSA. The tool’s answer is extensive, with each point backed by supporting bullets and footnotes. Here’s a screenshot of the intro…
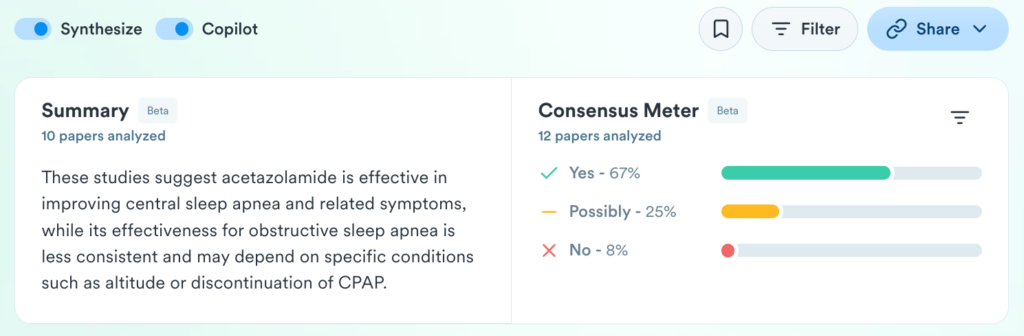
Each bullet is footnoted.
It happens that I had an unfilled prescription for a small quantity of acetazolamide (brand name Diamox) that I’d previously gotten in anticipation of a trip to Boulder, CO. At 5,400 feet, Boulder’s elevation doesn’t bother most people, but apparently CSA often is exacerbated by elevation. (Here’s Consensus’s take on the topic.) The Boulder trip got canceled, so based on the Consensus recommendation and a null search literature about Diamox causing any harm, I decided to start taking Diamox an hour or two each night before bed.
Since I started this experiment two weeks ago, my oxygen saturation has been consistently 96% or 97%. (Again, to jog your memory on how big an improvement this is, previously my SPO2 had gyrated between 92% and 96%, weighing in most nights at 94% or 95%.) Beyond the marked improvement in my nightly SPO2 average, I have experienced zero morning headaches, and, at night, no more jolting awake from dreams choked by agitation or confrontation. Doses that are four times higher than mine have tested safe when prescribed for at least six months. (The drug hasn’t been studied longer than that, likely because it’s off-patent and no drug company stands to reap windfall profits if acetazolamide is determined to be a miracle drug for say, I dunno, the 1-2% of US adults who have sleep apnea and are drifting towards Alzheimers.)
The disruption blueprint
Zooming way out, what might this anecdote about AI’s role in my own health journey possibly mean for the future of medicine?
It’s clear to me that AI will disrupt medicine and healthcare, not just augmenting traditional practices and institutions, but creating entirely new experiences and processes that supersede what exists today. When I say “disrupt,” I don’t just mean disturb or change. I mean utterly transform. This will happen according to a specific plot arc — disruptive innovation — we’ve seen enacted time and time again in the history of technology. In 1995, Harvard Business School professor Clay Christensen posited that a “disruptive innovation” starts life underpowered, cheap, outside traditional sales channels and serving customers whose needs aren’t met by existing solutions (or whose needs aren’t yet even articulated.) Eventually, the disruptive innovation spawns a new commercial ecosystem — new sales channels and consumer appetites — and migrates upward — in power AND the sophistication of the customer needs it serves — and obliterates incumbents.
Here’s the blueprint as described in Christensen’s 1995 paper in the Harvard Business Review:
In the history of the hard-disk-drive industry, the leaders stumbled at each point of disruptive technological change: when the diameter of disk drives shrank from the original 14 inches to 8 inches, then to 5.25 inches, and finally to 3.5 inches. Each of these new architectures initially offered the market substantially less storage capacity than the typical user in the established market required. For example, the 8-inch drive offered 20 MB when it was introduced, while the primary market for disk drives at that time-mainframes-required 200 MB on average. Not surprisingly, the leading computer manufacturers rejected the 8-inch architecture at first. As a result, their suppliers, whose mainstream products consisted of 14-inch drives with more than 200 MB of capacity, did not pursue the disruptive products aggressively. The pattern was repeated when the 5.25-inch and 3.5-inch drives emerged: established computer makers rejected the drives as inadequate, and, in turn, their disk-drive suppliers ignored them as well. But while they offered less storage capacity, the disruptive architectures created other important attributes – internal power supplies and smaller size (8-inch drives); still smaller size and low-cost stepper motors (5.25-inch drives); and ruggedness, light weight, and low-power consumption (3.5-inch drives). From the late 1970s to the mid-1980s, the availability of the three drives made possible the development of new markets for minicomputers, desktop PCs, and portahle computers, respectively. Although the smaller drives represented disruptive technological change, each was technologically straightforward. In fact, there were engineers at many leading companies who championed the new technologies and huilt working prototypes with bootlegged resources before management gave a formal go-ahead. Still, the leading companies could not move the products through their organizations and into the market in a timely way. Each time a disruptive technology emerged, between one-half and two-thirds of the estahlished manufacturers failed to introduce models employing the new architecture – in stark contrast to their timely launches of critical sustaining technologies.
To be clear, disruptive innovation isn’t just a blueprint that applies to the computer industry. Take, for example, the disruptive path of steamships to replace the prevailing transportation technology of 18th century, giant sail ships: “When steamships were introduced they were not reliable enough to travel trans-Atlantic distances, they couldn’t travel far without breaking down, and they were inclined to blow up. But steamships were able to find a niche in lake and river transport, where the distances were short, and where they had the advantage of being able to travel against the wind and on wind-still days. Once in the niche they could improve reliability until they were able to travel trans-Atlantic. Once that happened, all shipping switched to steam, and all the companies producing trans-Atlantic sailing ships went out of business; not one survived into the 20th century.” (Source.)
Maybe disruption’s avalanche begins with Consensus.ai (and peers)
With the disruptive innovation blueprint in mind, we can forsee that while AI may not replace doctors entirely — after all, they’ve got a powerful lobby and are deeply entrenched in our culture, laws, and health institutions — it will likely radically redefine what patients expect from them, starting in niches where traditional systems and practices fall short.
Unfortunately, as we all know, there’s lots of shortfall. The average doctor spends just 4 hours reading research per week, the average doctor’s knowledge is 17 years behind current research and best practices and most doctor’s visits clock in around 20 minutes. Doctors’ prescription habits are too often shaped by drug company promotions ranging from studies PHARMA finances to ads the drug makers buy in medical journals to brochures they distribute via drug reps. Laypeople’s access to best practices and medications that AI recommends will also boost demand for old, off-patent meds like acetazolamide that can play a transformative role in patients’ lives. Seriously people, if CSA and OSA might significantly boost your odds of Alzheimers and Parkinsons, why the hell aren’t doctors prescribing acetazolamide? Oh, right, no drug company will reap windfalls from the off-patent drug, and there are no drug reps pushing it. Any better reasons you can think of?
In the end, AI will disrupt healthcare just as it has other industries, not by replacing doctors outright, but by empowering patients to investigate their own solutions. This, in turn, will disrupt the value chains and marketing channels in which doctors are embedded: med schools, the FDA, EPIC, medical journals, drug company marketing infrastructure, and hospital systems. Tools like Consensus are just the beginning. They give us a glimpse of a future in which access to expert medical knowledge is democratized, forcing traditional and sometimes complacent healthcare gatekeepers to reach further, slash prices, and evolve quickly to meet consumer demand. The history of disruptive innovation — from tall sail ships to 5 1/4 inch disks — suggests the odds are heavily stacked against the incumbents.
Image source: https://commons.wikimedia.org/wiki/File:SS_Sirius_(1837).jpg
Update:
12/23/24 Superhuman performance of a large language model on the reasoning tasks of a physician: “In conclusion, o1-preview demonstrates superhuman performance in differential diagnosis, diagnostic clinical reasoning, and management reasoning, superior in multiple domains compared to prior model generations and human physicians. Given the pace of improvement of automated systems on medical reasoning benchmarks, better and more meaningful evaluation strategies are urgently needed. Performance of LLMs on challenging diagnostic problems indicate opportunities to leverage the models to support clinicians in real-world settings. Clinical trials and workforce (re)training with integrated AI systems are needed to confirm the potential of such systems to boost clinical practice and patient outcomes.”